And what can you do about it?
Gestational Diabetes is a form of diabetes (or high blood glucose) that develops in an expectant mother who previously did not have diabetes. During pregnancy, the placenta naturally produces hormones that can counteract the mother’s insulin, the hormone that your body needs to regulate your blood glucose (also known as blood sugar.) In some women, this can cause high levels of blood sugar, which can cause problems during pregnancy and down the road. It usually lasts from diagnosis through the end of her pregnancy.
Could I have Gestational Diabetes?
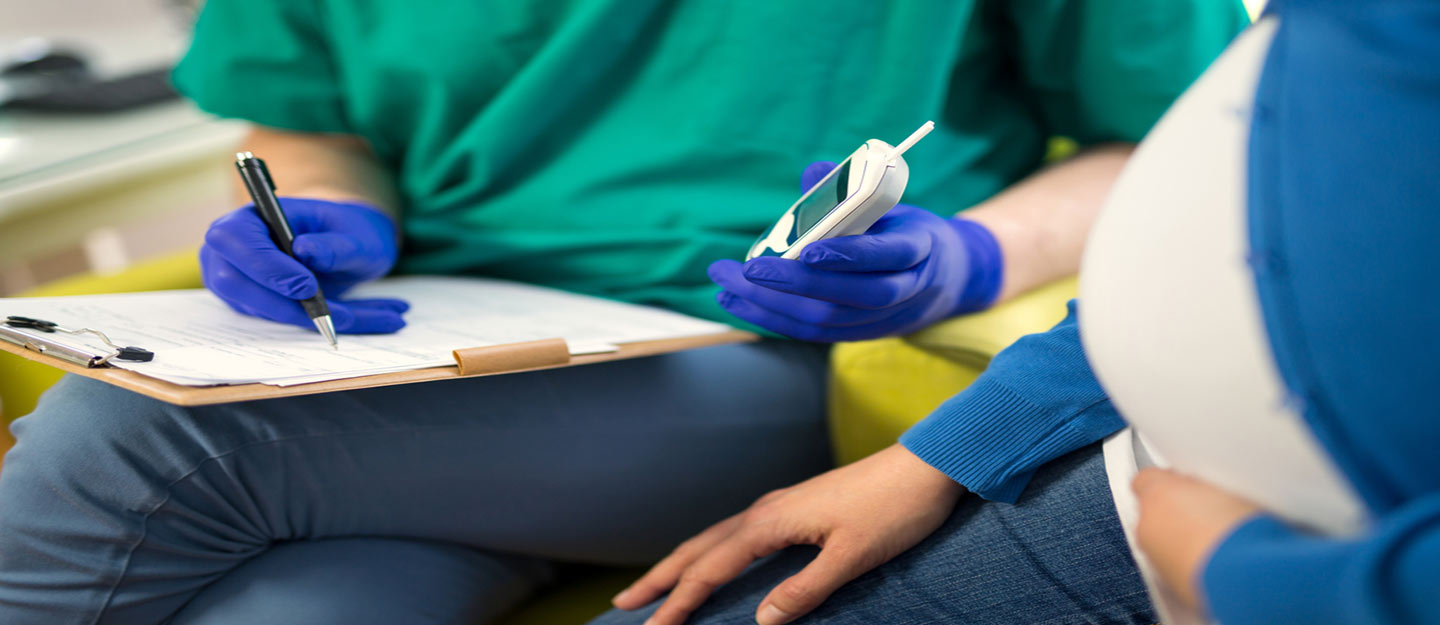
Get tested. During weeks 24-28 of pregnancy, you should see your health care provider to have your blood sugar checked. If you haven’t already, find a health care provider. During the initial glucose screening you will be asked to drink a sugary drink and wait for a period of time. After the wait, your blood sugar will be tested. If your results show a higher level of glucose than normal, they will have you do follow-up testing to determine whether or not you have Gestational Diabetes.
Can I prevent Gestational Diabetes?
Control your weight gain. Although no one knows exactly why Gestational Diabetes presents when it does, we do know that if you are overweight or obese you have an increased risk of developing it. So, the biggest thing you can do to prevent Gestational Diabetes is to focus on maintaining a healthy diet and exercise routine before and throughout your pregnancy. When pregnancy hunger strikes, try to stick to fruits, vegetables, lean proteins, low-fat dairy, and whole grains to fill you up.
Know if you are at risk. You are also at an increased risk if you have a family history of diabetes, are over 25 years old, or—for reasons which cannot be explained—are of non-Caucasian lineage such as Latina, Asian, Pacific Islander, African American, Alaska Native, or American Indian.
I’ve been diagnosed with Gestational Diabetes, what now?
Find a treatment plan.
First of all, do not panic. Gestational Diabetes is relatively common, reportedly occurring in as many as 18 percent of US pregnancies. Your health care provider will help you establish a treatment plan, which will likely include testing your blood sugar daily, and keeping up with a diet and exercise routine to help control your glucose. In about 10-20 percent of cases, insulin is needed to help mothers reach their glucose goals.
Monitor your baby.
Your health care provider will likely monitor your baby more closely now to watch for increased weight gain or respiratory problems. Since larger babies are more likely to have difficulty in childbirth, they may decide to induce you if you do not go into labor by your due date.
Follow-up for you and your child’s long-term health.
After your baby is born, it is important to follow up with your health care provider 6-12 weeks post labor to ensure that your blood sugar has returned to its normal levels. After that, you should have your blood sugar tested at least every three years as you now have an increased chance of developing type 2 diabetes. Also, ensure a healthy and active lifestyle for you and your child as he or she is now at increased risk for type 2 diabetes as well as obesity. Sign up for Healthy Futures to find the support you need to raise an active and healthy child in Michigan.